How Fluorescence can improve your dentistry.....and profitability
I have been using Fluorescence as an adjunct to visual examination and radiographs in my clinical practice for over 20 years. My introduction to the use of Fluorescence in my dental practice initially was with the Kavo Diagnodent , which I still use regularly. My current “go to” fluorescence source is now with the fully integrated, real time, system in my Zeiss Extaro 300 dental operating microscope. It is incredible how the consistent use of Fluorescence has improved the accuracy of my caries diagnosis by making it less subjective. In addition, we have incorporated the Fluorescence based Velscope into our practice as part of our oral CA screening regimen.
First, a short history of Fluorescence in dentistry. Fluorescence was first discovered in 1845 by Fredrick W. Herschel. He discovered that UV light can excite a quinine solution (e.g., tonic water) to emit blue light. Many decades later, in the early 1900s, the first uses of fluorophores in biological investigations were performed to stain tissues, bacteria, and other pathogens. This was later developed into fluorescence microscopy by Carl Zeiss and Carl Reichert. In dentistry, journal articles citing laser fluorescence are available from the mid 1980’s and the Kavo Diagnodent, based on laser-induced Fluorescence, was introduced in the early 2000’s. A recent Medline search with search terms Fluorescence and caries yielded over 800 results!
Dental equipment using Fluorescence is covered by the Food and Drug administration under Part 872- Dental Devices Subpart B- Diagnostic devices, Sec. 872.1745 Laser fluorescence caries detection device. This section states: A laser fluorescence caries detection device is a laser, a fluorescence detector housed in a dental handpiece, and a control console that performs device calibration, as well as variable tone emitting and fluorescence measurement functions. The intended use of the device is to aid in the detection of tooth decay by measuring increased laser induced fluorescence. |
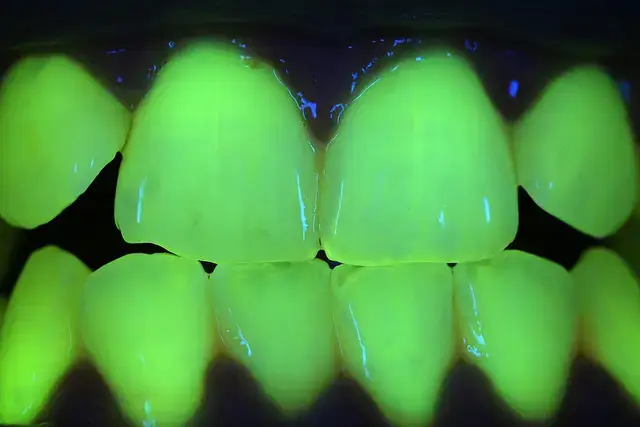
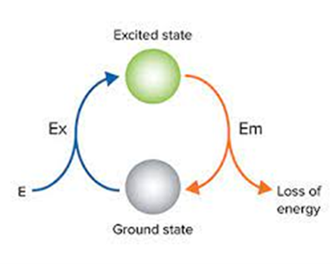
The science of Fluorescence is based on the absorption of light and reemitting at a different, longer, wavelength. Porphyrins in bacteria found in caries will absorb and re-emit fluorescent light in the blue-green wavelengths. Typical emitted wavelengths are in the 405-500 nm range (blue green and red) and are absorbed by porphyrin-induced metabolites produced by oral microorganisms in dental caries and dental plaques and re-emitted at longer wavelengths typically appearing as red, pink or yellow when viewed in a monitor or microscope.
Healthy enamel and dentin re-emit in the greenish blue range, so it is very easy to distinguish healthy tooth structure from caries affected or infected hard tissues. This is very useful for detecting caries, fractures, and calcified canals. Furthermore, there is some quantifiable difference in the quality of the absorbed and re-emitted light giving clues about the severity of the decay and even inferences on depth of decay can be made. Existing composite restorations also fluoresce making it easy to distinguish between existing restorations and tooth structure.

Pretreatment of Tooth #14 – Note clinically evident recurrent caries.

Tooth #14 following initial preparation and caries excavation. Healthy enamel and dentin (green blue), existing composite (lighter green, yellow), caries (affected dentin in shades of orange) and soft caries (infected dentin in darker orange red)
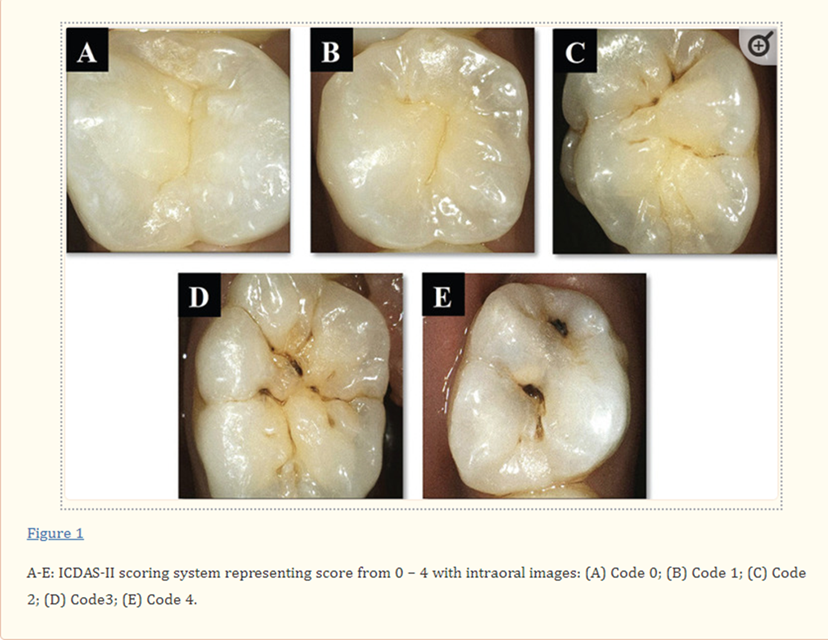
Historically, caries detection has been via visual identification and radiographs. Additional methods include transillumination and caries staining techniques. In general, visual inspection is the simplest and most commonly used method for detecting caries in the clinical setting. Unfortunately, reliable, and consistent visual detection is possible only after the lesion has progressed significantly to the dentin and classification of caries lesions remains elusive. Recent efforts to reclassify surface caries have been tried in the form of the ICDAS system currently taught in most dental programs. Radiography, which has long been used as a traditional diagnostic method, is considered unreliable for quantitative diagnosis due to its low sensitivity in detection of early carious lesions and variations in sensor quality.
Currently, the American Dental Association (ADA) discourages the use of routine radiographic examinations for screening purposes due to the inherent risks of radiation exposure. Transillumination using visible light can be useful for interproximal caries detection and particularly fracture diagnosis. However, transillumination is unreliable and inconsistent for qualitative and quantitative interproximal caries diagnosis. Further caries identification can be accomplished with caries detecting chemical dyes. Both transillumination and caries detecting dyes are limited by operator error and lack of standards for quantification.
In the past few decades adjunctive diagnostic techniques utilizing Fluorescence, such as quantitative light-induced fluorescence (QLF), optical fiber-transmitted illumination using visible light, DIAGNOdent using laser induced fluorescence, and, most recently, blue green emitting fluorescence sources commercially available by various manufacturers.
In my practice, Fluorescence is used routinely for caries, fracture, and calcified canal identification, and CA screening. The most prevalent use is for caries identification, especially intraoperatively during restorative dentistry procedures. Typically, I will use Fluorescence following initial outline preparation and caries excavation to insure removal of “infected” or soft carious dentin. I will generally leave “affected” or stained dentin and treat with chlorhexidine scrub. Often, even after thorough caries excavation I will find additional caries using Fluorescence that must be removed prior to final restoration. This is a huge advantage and provides a significant benefit to my patients in longer-lasting restorations. If not for Fluorescence I would not have seen the additional caries. It is true that I could use caries staining dye; however, this requires significant additional time, preparation, and can be a mess.
I also routinely utilize my Kavo Diagnodent (www.Kavo.com) for screening and diagnosis of pit and fissure caries.
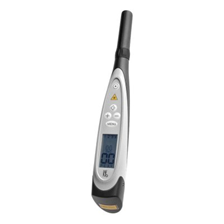
Kavo Diagnodent
The Diagnodent uses laser fluorescence to aid in the detection of caries within the tooth structure. As the incident laser light is dispersed into the site, carious tooth structure will exhibit fluorescence, proportionate to the degree of caries, resulting in elevated scale readings on the display. Clean healthy tooth structure exhibits little or no fluorescence and will result in very low scale readings on the display.
We are often faced with a dilemma when diagnosing incipient lesions in occlusal pits and fissures. This is partially addressed in the ICDAS system of occlusal caries classification (see image). There is universal agreement that ICDAS 3 and 4 lesions should be repaired; however, the decision of whether to monitor or restore ICDAS 1 and 2 lesions often rests with the subjective prejudices of the clinician without objective or quantifiable assessment criterion. The Diagnodent is an excellent adjunctive diagnostic aid in that it provides an arbitrary but quantifiable and consistent numeric (0-100) assessment of caries depth (provided the unit is properly calibrated and maintained). Furthermore, the clinician can decide at what level of numeric outcome he or she feels comfortable with restoring vs observation. For example, we typically will not restore lesions with less than a 30-35 score. The Diagnodent also emits an audible tone that increases in frequency as the test number increases. This certainly helps with case presentation and creating a sense of urgency for the patient!

18x magnification image ICDAS 1-2 lesion in distal pit of tooth #29. Note Zirconia crown #30

Florescence 11x magnification image tooth #29. Note Florescence in mesial and distal pits and Zirconia crown does not floresce.
Accurate and consistent diagnosis of recurrent caries around dental restorations has always been a clinical challenge for dentists. Fluorescence can make the decision of replacing or watching an older restoration less subjective. The addition of Fluorescein dye to document failing restoration margins can also add an additional diagnostic regimen to the clinician’ regimen and help with the restorative decision process.

Tooth #30 with older amalgam restoration. Is the lingual margin leaking?
Tooth #30 with addition of Florescein dye on lingual margin. Note dye is pooled in margin and fluorescing.
One of the more frustrating clinical situations for general dentists and endodontists is fracture identification. Fractures, and especially pulpal floor fractures, rarely show up on radiographs and are very difficult to see clinically unless staining has occurred. Under Fluorescence, fractures become readily discernable. The use of Fluorescein dye, used in optometry to diagnose corneal fractures, can be added to enhance the fracture. This can also be used to help communicate the presence of fractures to our friends at insurance companies who will often debate the presence or absence of pathologies requiring treatment.
The ability to identify pulpal floor fractures during endodontics is essential for determining prognosis and consulting with the patient about whether treatment should be continued with lower chance of endodontic success or abandoned, and extraction performed. The added medical-legal benefit of a permanent photographic record cannot be ignored.

Image of pulpal floor under 11x magnification with no evident fracture.

The same pulpal floor under Florescence showing fracture (thin orange line)
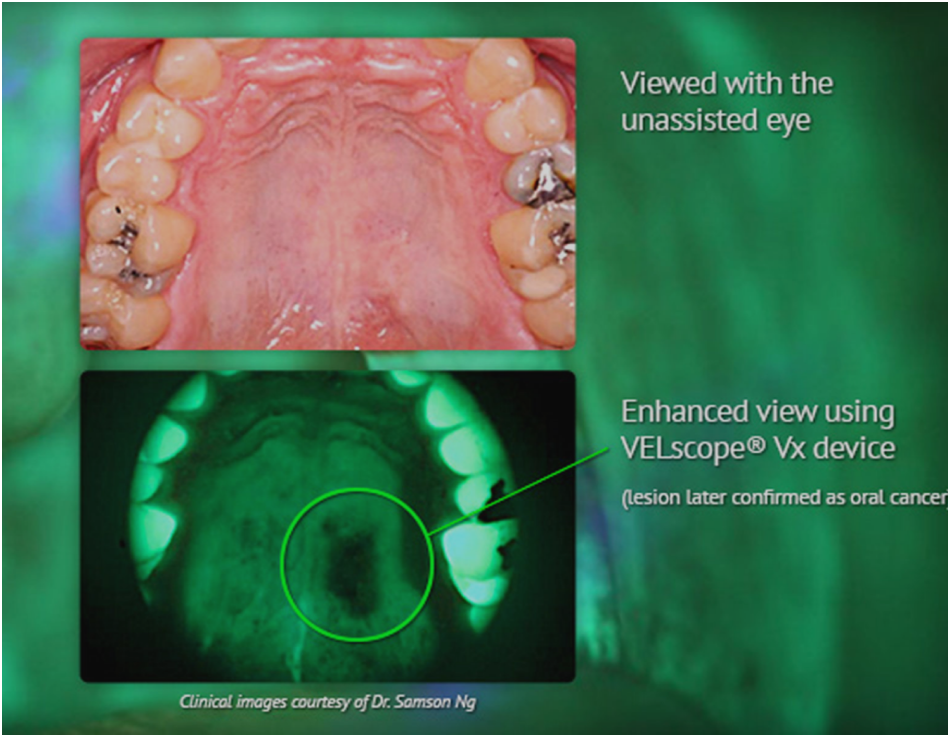
An additional use of Fluorescence is with CA screening and diagnosis. We have made an investment in oral CA screening with the purchase of a VELscope (www velscope.com). Although the VELscope uses a blue LED light source The VELscope uses relies on the principle of tissue fluorescence rather than reflectance. Tissue fluorescence is caused by fluorophores, which are chemical compounds that react to light excitation. When exposed to the blue light of the VELscope, fluorophores respond by emitting their own light at a longer wavelength, which can be observed via the optical filter in the VELscope eyepiece. It’s the excitation of fluorophores, or lack thereof in some instances, that enables the VELscope to visualize cellular change in the oral mucosa.

VELscope
There are several commercially available FDA approved systems available in today’s marketplace. These can be separated into direct, meaning the fluorescent light source is incorporated into the optical device, either a microscope or loupes, or indirect, where the clinical image is transmitted to a computer or laptop and viewed on the monitor. Direct systems have the huge advantage in that they can be used “real-time” intraoperatively while actually excavating caries. Indirect systems require checking the monitor for caries, returning to the patient for caries removal, and again imaging the area to see if caries remains. This can take several steps and adds significant time to the restorative procedure.
Without question the most effective fluorescent systems are incorporated into dental operating microscopes. Microscopes (and loupes where available) can concurrently identify caries and the tooth treated and restore as needed – this is termed Theragnosis. Currently, there are only two FDA approved fluorescence systems integrated into a dental operating microscope, the Zeiss Extaro 300 https://www.zeiss.com/meditec/en/products/surgical-microscopes.html#dental-treatments and CJ Optik Flexion www.synca.com. I use the Zeiss Extaro 300 microscope system in my practice. As previously stated, the ability to use Fluorescence in real time is an incredible advantage as the following video will show.
For above video, please note: The Fluorescence Mode is intended to be used by dentist as an aid in the detection of dental caries. Treatment of caries under Fluorescence is not currently approved by the FDA. Clinicians should use Fluorescence for caries removal at their own discretion and inform and obtain approval from the patient.
The ability to identify and quantify caries, healthy tooth structure, and existing composite restorations at one time is game changing and creates incredible clinical efficiency when the ability to simultaneously treat (Theragnosis) is added.
There is one loupe-based fluorescent system available in the U.S. through Designs for Vision. The loupe-based system has the common advantage of being real-time; however, it suffers from lower magnification levels and more weight increasing stress on the bridge of the nose and head and neck.

Loupe-based florescent system available through Designs for Vision.
There are several indirect fluorescence light source options; however, some are not available in the U.S. or are difficult to get. The indirect fluorescence systems work much like an intraoral camera and project their images on a computer screen or television monitor. I have listed a few of the available systems and the light source used for caries detection. There are other systems available, but space restricts listing to the most popular systems in each category.
QLF or Quantitative Light Induced Fluorescence. This system uses light with wavelengths around 405 nm to excite yellow fluorescence at wavelengths above 520 nm. Its diagnostic capacity is based on the mechanism that the intensity of natural fluorescence of a tooth is decreased by scattering due to a caries lesion.
Inspektor Pro QLF Camera system has been approved by the FDA and is available for dental professionals and research and educational institutes in several countries. It is a very bulky system potentially better suited to university or research applications. The QRay pen is available from QLF Technologies www.qlftechnology.com.
Cariescan Pro. The CarieScan PRO™ uses ACIST (AC Impedance Spectroscopy) technology to quantify dental caries measuring changes in tooth mineral density. It is available at www.eclipse-dental.com.
Air Techniques CAM X Spectra Is an LED Fluorescence system. It uses a small detecting wand similar to an intraoral camera and projects images on a PC monitor or laptop. www.airtechniques.com/product/camx-spectra-caries-detection-aid.
Let’s discuss return on investment (ROI). My clinical experience with Fluorescence is with Kavo Diagnodent and Zeiss Extaro 300 microscope. It is my opinion that any Fluorescence system will pay for itself and provide a positive direct and indirect ROI very soon. A typical clinical scenario in my practice is the patient will have a carious lesion diagnosed at their hygiene appointment and a restoration will be treatment planned. At the clinical appointment I will typically scan the tooth and area after removing the existing restoration (if there is one) and visible caries. This is the end of the preparation process for most dentists and restorative therapy will then commence. In my office I will scan the prepared tooth using Fluorescence Mode in my microscope. Often, I will find additional caries that results in the tooth requiring additional surface preparation, and thus a different ADA code, resulting in a higher fee. Often, I will find previously undiagnosed caries on adjacent teeth. I can then use the intraoral imaging camera and display the caries on my iPad and amend the treatment plan. I have never had a patient refuse treatment. Also, I occasionally change a treatmnent plan from direct restorative to a full coverage indirect restoration based on Fluorescence imaging. Even if the patient does not accept the recommended full coverage restoration, I have images that can be part of the permanent clinical record and make operative notes that a crown was recommended. Then in a few years if the restoration breaks I have clinical notes and evidence that a crown was recommneded. Priceless! Additionally, the ADA has a code, American Dental Association Billing Code D0600 “Non-ionizing diagnostic procedure capable of quantifying, monitoring, and recording changes in structure of enamel, dentin and cementum.” I do not charge for Fluorescence examination but feel it is very reasonable for a clinician to charge based on the capital expense of the equipment and additional time required. Whether insurance companies will reimburse is a question for another article.
I also believe there is indirect ROI. As this is not a mainstream dental technology and not often found in dental practices there is an element of the “Purple Cow” perception. Patients do recognize when you have invested in technology beyond the norm and will tell friends and relatives, potentially adding new patients without direct marketing costs.
In conclusion, there is a wonderful world of caries diagnosis using Fluorescence. I encourage every clinician to investigate this wonderful technology. There is a system that will work in any office and budget.
Feel free to contact me directly if you have any questions at: drglenn@hobsondental.com