Why Perio Protect?
Systemic and localized antibiotic therapies have been used for decades to treat patients with periodontitis and they have not been particularly successful. 47% of Americans aged 30 and older have periodontitis. By the time we reach 65 years, 70% of Americans have the disease. (i) If antibiotics worked well, our incidence of disease would be significantly lower.
Biofilm-based diseases – chronic periodontitis is a classic biofilm-based disease – are refractory to antibiotics. (ii) Our continual reliance on antibiotics only makes the problem harder to treat. This is true for all health professions. The more antibiotics we use, the more resistant bacteria become. The situation is so dire that the Centers for Disease Control and Prevention has proclaimed this the post-antibiotic age. (iii)
Superbugs, bacteria that have become resistant to antibiotic drugs, (iv) pose real health risks. Not only might a patient need several rounds of antibiotics to recover from an infection, but the infections that become more difficult to treat also increase the risk of disease transmission to others, of more severe illness, higher health care costs, adverse events like Clostridioides difficile (C Diff) infections, and death. (v)
Dental prescriptions for antibiotics have been directly linked to C Diff infections in patients.(vi) Dentists are the third highest prescribers of antibiotics in outpatient settings and the number one prescriber in outpatient settings of clindamycin, a drug associated with the highest risk of C Diff infections. (vii) 500,000 people in the US face C Diff infections each year, (viii) and 15% of them die within the first 30 days. For survivors, 25-30% are reinfected after initial recovery. It is often a long, debilitating recovery.
It is worth thinking carefully about antibiotic prescribing habits, especially concerning clindamycin, and about alternatives to antibiotic treatment.
When it comes to periodontal health, it is imperative that we have effective treatment options for the post-antibiotic age, but the first focus is diagnosis. This key component of care is often neglected. (ix) Do a simple chart audit to get a glimpse of the situation in your own office. You might also consider some charting software like Florida Probe’s VoiceWorks (x) to reveal more clearly the gingival conditions to patients and to generate graphs that help you track patient health over time.
Chronic periodontal disease results from chronically infected oral wounds and associated inflammation. Debridement and the physical removal of deposits deep below the gums provide acute wound care. That is often insufficient to put periodontitis into remission and prevent its reoccurrence. For long-term success, you need additional treatment. And that treatment is needed at home.
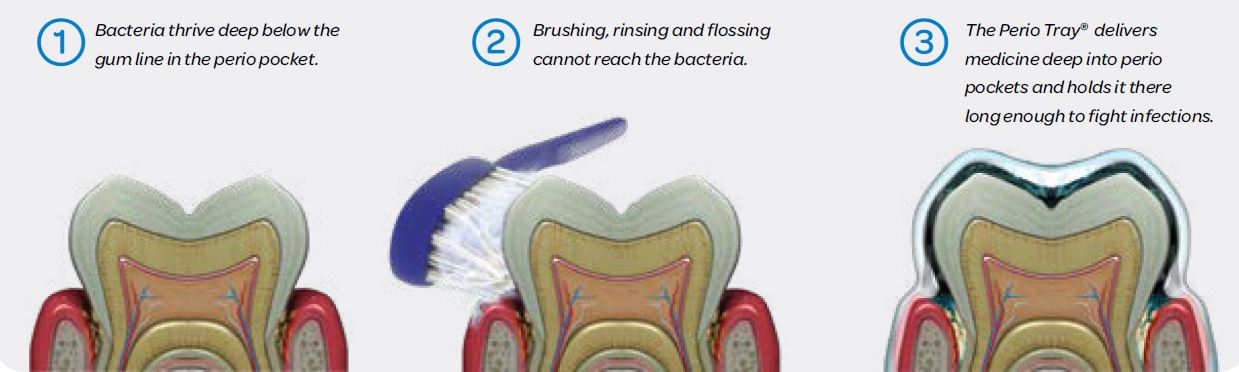
Toothbrush, rinse, and floss do not get deep enough below the gums for effective disease management between office visits. Patients benefit from Perio Tray™ therapy (Perio Protect) because it applies gentle pressure (compression) against edematous gingival tissue and it also delivers an oral debriding and oral wound care agent, hydrogen peroxide gel, deep into the periodontal pocket. Held in place with Perio Tray™ delivery, the peroxide debrides the wounds, decreases bacterial loads, and changes the microenvironment of the periodontal pocket via the release of oxygen from the peroxide. The Perio Tray™ internal peripheral seal traps the oxygen within the tray and deep under the gums, creating a toxic environment for anaerobes and the right environment for healthy bacteria to repopulate. (xi)
 With daily Perio Tray™ applications of 1.7% hydrogen peroxide gel (Perio Gel™) in 10–15-minute increments, there are substantial reductions in bleeding, inflammation, and pocketing. Controlled clinical trials testing adjunctive Perio Tray™ therapy with scaling demonstrate significantly better reductions in bleeding and pocketing than scaling alone. (xii) This improvement in oral health is important for patients’ general health and wellness.
With daily Perio Tray™ applications of 1.7% hydrogen peroxide gel (Perio Gel™) in 10–15-minute increments, there are substantial reductions in bleeding, inflammation, and pocketing. Controlled clinical trials testing adjunctive Perio Tray™ therapy with scaling demonstrate significantly better reductions in bleeding and pocketing than scaling alone. (xii) This improvement in oral health is important for patients’ general health and wellness.
Periodontal disease puts a chronic, low-grade inflammatory burden on the immune system. To help patients understand this, you might compare the immune system to a battery. The more things hooked up to the battery, gum disease and type 2 diabetes for example, the quicker the battery is drained. Let’s unplug gum disease from the immune system battery so that the body can work more efficiently on other systemic inflammatory conditions. In this light, dental care is vital for patient health and wellness.
Offices that put their patients’ health first will be profitable. Hygiene-driven dentistry like Perio Protect is proactive, with a focus on early intervention for healthier patients. This approach has long-term financial benefits for your patients and for your practice because so many patients need this help. For your patients with gingivitis and early stages of periodontal disease, improving gum health to prevent the loss of bone is a good and realistic goal with Perio Tray™ therapy. You can also help your maintenance patients stay so healthy that they do not need as much repetitive care. For patients who cannot avoid surgery, you can maintain your surgical gains with Perio Tray™ therapy for long-term health, including saving more natural teeth. For patients with implants, it is important to prevent and address peri-implant mucositis or peri-implantitis. You can do this well with Perio Tray™ therapy. (xiii)
The Perio Tray ™ is the only prescription periodontal medicament carrier with specific FDA clearance for deep delivery into the periodontal pocket and with clinical trials and research to support treatment claims. It provides proven, effective homecare for the post-antibiotic age.




