Daniel and his wife Sara were both patients of mine. When Sara was in for an appointment, she was sharing with my hygienist that Daniel snored. She was frustrated because his snoring had reached a level that now disrupted her own sleep. Sara had recently seen a social media campaign I’d done on mouth breathing, and she had a lot of questions, especially as Daniel’s snoring had gotten worse.
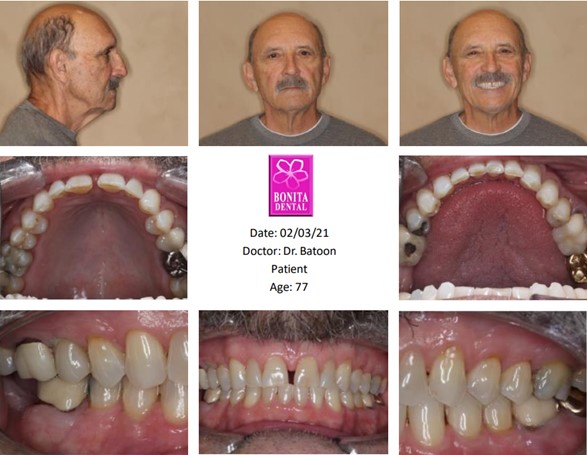
Daniel was 77 years old and although he’d been previously diagnosed with cardiovascular arrythmia, he seemed healthy in every other aspect. He exercised 2-3 times a week, had a healthy BMI, and was a vegetarian. He was actually in amazing shape.
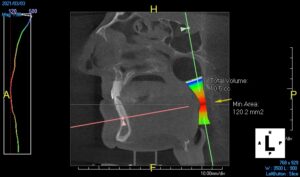
Narrow Airway
At Sara’s urging, Daniel scheduled an appointment with me to discuss the snoring. I had previously sent him a sleep questionnaire (Epworth Sleepiness Scale) and his score results were unremarkable. Besides filling out a STOP BANG form which was positive for snoring, nothing was alarming in his medical history intake form. I sent him to a sleep physician for consultation only to find out his polysomnography test resulted in the following: severe snoring with an AHI of 36.
AHI, which stands for apnea/hypopnea index, is the current measurement that the medical community follows to assess severity of sleep apnea and strategy for treatment. Daniel was put on CPAP because his titration study showed marked improvement with CPAP use. Today his AHI with CPAP is managed at 1.2. So, what does that translate to?
Compared to before CPAP, his heart is not working as hard every night. His snoring is completely resolved, and he probably improved his lifetime span with a guarantee of 10 years. It may be difficult to imagine being tethered to a tube with a mask or nosepiece every night, but the benefits outweigh the risks. Daniel’s quality of life improved and his bed partner just got an upgrade in her quality of sleep. If he hadn’t taken action and made an appointment, and if I decided that screening for airway was not part of my dental examination, then he might not be sitting in my dental chair for 10 more years.
The COVID–19 pandemic caused the dental community to change their protocols in 2020. Just like the epidemic of oral cancer and periodontal disease have changed the way we practice, dentistry had to pivot. As clinicians, we must pivot. Maybe it sounds corny or pretentious to imagine that as dental providers we would make the time to change our workflow. Are we changing our workflow, or are we improving our workflow to be more caring professionals? I believe it to be the latter. Sure, high technology in dentistry matters, as does hiring and training our team to be skilled and competent in procedures. Yet, what also matters is that patients feel committed to the care they receive so that when we recommend a procedure, our case acceptance and, of course, payment for services rendered move to conversion and completion.
Screening for airway involves a simple questionnaire and asking the questions that involve more clarification. It also involves evaluating soft tissues, dental malocclusions, TMJ and craniofacial properties. Evidence based dentistry supports that 52% of TMJ patients may also have sleep-related issues. (1)
Snoring also is a symptom of sleep related breathing disorders and age does not discriminate. Women and children are part of this demographic and may not be loud snorers but loudmouth–breathers. Although the incidence of sleep apnea in children is known to be 1-4%, adenoid and tonsil hypertrophy have been a common risk factor. (2)
Yet, after A&T surgery, adenoid tissue regrowth is about 8%. This was due to allergic rhinitis or upper airway obstruction (3)
Mouth-breathing does not improve and inflammation around those areas has increased. What is more important is that screening for airway can validate symptoms of bruxism, scalloping of the tongue, teeth fractures and malocclusions. As a dentist, we can be more aware of a systemic relationship such as sleep apnea to oral manifestations. It is never too late to be more proactive in our workday. Just a little more follow-up or asking qualifying questions can save a life. You just don’t know how (or when) your moment of caring can save a life.
References
- (1) Sanders AE, Essick GK, Fillingim R, Knott C, Ohrbach R, Greenspan JD, Diatchenko L, Maixner W, Dubner R, Bair E, Miller VE, Slade GD. Sleep apnea symptoms and risk of temporomandibular disorder: OPPERA cohort. J Dent Res. 2013 Jul;92(7 Suppl):70S-7S. doi: 10.1177/0022034513488140. Epub 2013 May 20. PMID: 23690360; PMCID: PMC3706181.
- (2) James L. Goodwin, Monica M. Vasquez, Graciela E. Silva, Stuart F. Quan, Incidence and Remission of Sleep-Disordered Breathing and Related Symptoms in 6- to 17-Year Old Children—The Tucson Children's Assessment of Sleep Apnea Study, The Journal of Pediatrics, Volume 157, Issue 1,2010,Pages 57-61,ISSN 0022-3476, https://doi.org/10.1016/j.jpeds.2010.01.033. https://www.sciencedirect.com/science/article/pii/S0022347610000491)
- (3) Paramaesvaran S, Ahmadzada S, Eslick GD. Incidence and potential risk factors for adenoid regrowth and revision adenoidectomy: A meta-analysis. Int J Pediatr Otorhinolaryngol. 2020 Oct;137:110220. doi: 10.1016/j.ijporl.2020.110220. Epub 2020 Jul 11. Erratum in: Int J Pediatr Otorhinolaryngol. 2021 Oct;149:110885. PMID: 32896343.