Identifying Signs of Mental Health Issues in the Dental Setting
Suicide remains a leading cause of death globally, with over 700,000 people dying by suicide annually (World Health Organization, 2021). Research indicates that mental health disorders, particularly depression and anxiety, are critical risk factors for suicide (Nock et al., 2018). Oral health professionals, especially dentists, often encounter patients regularly for preventive and curative care, positioning them uniquely to identify early signs of mental health issues that may contribute to suicidal ideation.
The concept of oral systemic health emphasizes the interconnections between oral health and overall systemic health, including mental health. Studies have shown that oral health can reflect broader health issues, including psychological conditions (Warren et al., 2017). Given this intersection, there is an emerging recognition of the potential role dentists can play in identifying and supporting patients at risk of suicide.
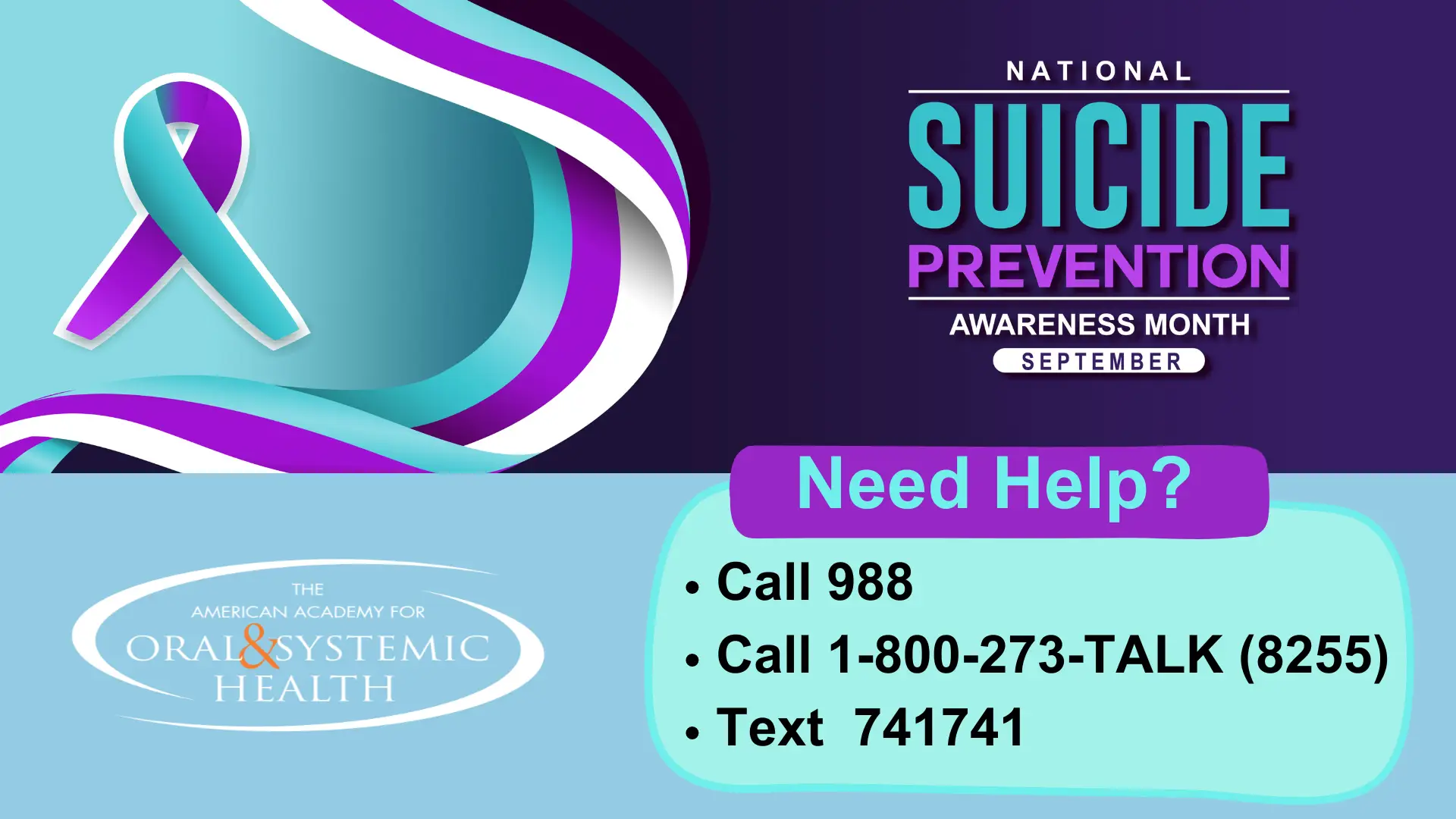
Please print this and post it in your office!
The Oral Systemic Connection and Mental Health
The relationship between oral health and mental health is well-documented. Poor oral health is often associated with psychological distress and mental health conditions like depression and anxiety (Gibson et al., 2020). For instance, patients with mental health disorders may neglect oral hygiene due to low motivation, leading to conditions such as dental caries and periodontal disease (Johannsen et al., 2016). Conversely, chronic dental pain and tooth loss can exacerbate feelings of hopelessness and despair, potentially contributing to suicidal thoughts (Santos et al., 2022).
Additionally, certain psychotropic medications used to treat mental health disorders can lead to xerostomia (dry mouth), increasing the risk of dental decay and periodontal disease (Friedlander & Mahler, 2001). This bidirectional relationship underscores the importance of an integrated approach to health care, where dentists are aware of their patient’s mental health status and collaborate with mental health professionals to provide comprehensive care.
Identifying Signs of Mental Health Issues in the Dental Setting
Dentists and dental hygienists are often among the first health professionals to notice signs that may indicate a patient is struggling with mental health issues. These signs include poor oral hygiene, signs of self-inflicted oral injuries, significant weight loss or gain affecting oral health, and a flat affect or lack of responsiveness during dental visits (Friedlander & Marder, 2002).
Moreover, dentists are well-positioned to recognize signs of anxiety and depression. Dental anxiety is a common condition that affects up to 20% of the population and can often overlap with generalized anxiety disorders (Humphris et al., 2013). By carefully observing patients’ behaviors and responses, dentists can identify individuals who may need further mental health evaluation.
The Role of Dentists in Suicide Prevention
Dentists can play a pivotal role in suicide prevention through several strategies:
- Mental Health Training and Education: Dental professionals should receive training to recognize the signs and symptoms of mental health disorders and suicidal ideation. Enhanced mental health literacy among dentists can improve their ability to identify at-risk patients and refer them to appropriate mental health services (Kakoulidou et al., 2020).
- Routine Screening for Mental Health Issues: Integrating mental health screenings into routine dental visits can help identify patients who may be at risk. Simple tools like the Patient Health Questionnaire-2 (PHQ-2) or Generalized Anxiety Disorder-2 (GAD-2) can be used as part of the dental assessment to screen for depression and anxiety (Spitzer et al., 2006).
- Creating a Supportive Environment: Dentists can create a safe and non-judgmental environment for patients to discuss their mental health concerns. Building rapport and trust can encourage patients to open up about their struggles, allowing for timely intervention (Little et al., 2018).
- Referral to Mental Health Professionals: Dentists should establish a network of mental health professionals for timely referrals. A multidisciplinary approach is crucial in managing patients at risk of suicide, ensuring they receive comprehensive care (Petersen et al., 2005).
- Monitoring and Follow-Up: Dentists can also play a role in monitoring at-risk patients over time. Regular dental visits provide opportunities for ongoing assessment and support, ensuring patients remain connected to care networks (Johnston et al., 2019).
Barriers and Challenges
Despite the potential role of dentists in suicide prevention, several barriers exist. These include a lack of training in mental health, time constraints during dental appointments, and concerns about patient privacy and stigma associated with mental health discussions (Walsh et al., 2013). Additionally, there may be a lack of established referral pathways to mental health services, making it challenging for dentists to connect patients with the care they need.
Conclusion
Dentists, as frontline health professionals, have a unique opportunity to contribute to suicide prevention efforts. By recognizing the signs of mental health issues, providing supportive environments, conducting routine screenings, and collaborating with mental health professionals, dentists can play a significant role in identifying at-risk patients and preventing suicide. Further research is needed to explore the most effective strategies for integrating mental health care into dental practice and overcoming existing barriers to implementation.
AAOSH Resources
Mental health and psychological issues are covered across the AAOSH Core Curriculum. We hope you will enjoy this sample course from our core curriculum. (Please Note: This is a sample course; watching this video here does not provide CE credit. Please visit members.aaosh.org to search for these courses and earn CE credit.) https://youtu.be/yU0Ae6jHXC4
Join AAOSH today! Click here to learn more about joining our organization! Use the code TPD30 and save 30% off your membership!
References
Friedlander, A. H., & Mahler, M. E. (2001). Major depressive disorder: psychopathology, medical management and dental implications. Journal of the American Dental Association, 132(5), 629-638.
Friedlander, A. H., & Marder, S. R. (2002). The psychopathology, medical management and dental implications of schizophrenia. Journal of the American Dental Association, 133(5), 603-610.
Gibson, D. S., Amarasena, N., & Kumar, S. (2020). Oral health status and hygiene habits of patients with mental disorders: A comprehensive review. Australian Dental Journal, 65(4), 292-300.
Humphris, G., Crawford, J. R., Hill, K., Gilbert, A., & Freeman, R. (2013). UK population norms for the modified dental anxiety scale with percentile calculator: Adult dental health survey 2009 results. BMC Oral Health, 13(1), 1-6.
Johannsen, A., Rydmark, I., & Söderfeldt, B. (2016). Effects of patients’ anxiety, depression and behavior on oral health and treatment outcome: A patient perspective. BMC Oral Health, 16(1), 3-12.
Johnston, C., Clement, S., & Humphris, G. M. (2019). Mental health problems and dental service attendance: A systematic review. British Dental Journal, 226(9), 689-698.
Kakoulidou, T., Margaritis, V., Kakoulidis, S., & Kakoulidou, M. (2020). The dentist’s role in detecting and managing mental health disorders. European Archives of Paediatric Dentistry, 21(6), 713-722.
Little, J. W., Miller, C. S., Rhodus, N. L., & Dahlen, G. (2018). Dental Management of the Medically Compromised Patient. Elsevier Health Sciences.
Nock, M. K., et al. (2018). Suicide and suicidal behavior. Epidemiologic Reviews, 40(1), 139-154.
Petersen, P. E., Kwan, S., & Ogawa, H. (2005). The role of oral health in promoting quality of life. Quality of Life Research, 14(3), 55-61.
Santos, L. F., Costa, P. S., & Ferreira, E. F. (2022). Oral health and mental health: A case-control study of Brazilian adults. Community Dentistry and Oral Epidemiology, 50*2), 106-114.
Spitzer, R. L., Kroenke, K., Williams, J. B., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092-1097.
Walsh, L., Brooker, C., & Elston, S. (2013). Influence of psychiatric history on patients’ attitudes to dental care. BMC Oral Health, 13(1), 1-6.
Warren, K. R., & Naghavi, M. (2017). Depression and oral health: A bidirectional association. Journal of Affective Disorders, 221, 297-305.
World Health Organization. (2021). Suicide worldwide in 2019: Global health estimates. World Health Organization.



