Article co-authored by Timothy Kosinski DDS, MAGD and Stephanie Tilley, DMD.
Dental implants have become a prominent mode of therapy to replace missing teeth with functional and esthetic restorations. Teeth that are deemed non-restorable are extracted in preparation for future dental implants. All practitioners are aware of the consequences of tooth loss over time, as the hard tissue tends to reduce both horizontally and vertically. This may become a challenge to future dental implant placement in the posterior mandible where the main concern is impingement on the mandibular nerve, resulting in paresthesia, and the posterior maxilla, where the maxillary sinus itself may have collapsed. (1) The bone loss may make implant placement challenging, or not possible without more invasive and expensive surgical grafting procedures.
Root canal therapy has been a long- accepted method of retaining damaged or infected dentition. In some cases, the therapy may fail, or the infection may recur after a time. Sometimes the RCT can be retreated, but if not possible, another option is referred to as an apicoectomy. Root canal therapy can be complicated in some particular teeth, such as molars and bicuspids. Parts of roots could fracture, perforations can occur, apical lesions can persist, or canals can be missed in treatment. Infection may ensue, resulting in an abscess apparent on digital radiographs, CBCT analysis and draining fistulas visualized intraorally. The options for the practitioners include extraction of the compromised tooth, or an attempt to salvage the tooth. (2)
An apicoectomy is simply a root-end resection and removal of the granulation tissue causing discomfort and drainage. A tissue reflection is made elucidating the diseased site. The area is cleaned using sharp curettes, a surgical bur to remove root structure and/or laser therapy to attempt to sterilize the spot. Several techniques have been used following this, including condensing a small filling to seal the end of the root canal. There are many materials used as root-end filling materials, but there is no complete agreement on the ideal material to be chosen. Amalgam, IRM, EBA, ZOE and MTA paste are a few of products often attempted. Eugenol in any of these materials seems to cause irritation. (3) MTA is a mineral trioxide aggregate based, salicylate resin root canal sealer which is prominently utilized. Following placement, sutures are utilized to reposition the flap and the surgical area is allowed to heal. Such treatment may be an effective means to salvage the tooth in function. However, some literature states a success rate of approximately 62%. (4,5)
There are many biomaterials used in bone grafting socket sites following tooth extraction. When one considers all the subcategories there are hundreds of products on the market. Hydroxyapatites, Tri-Calcium Phosphates, and other Calcium Phosphates are promoted. (6,7) Autografts and allografts are other material options. Osteogen (Impladent) is a significant synthetic grafting material. It is a Calcium deficient apatite similar to the mineral in human bone allograft. Osteogen is bioactive in that it controls soft tissue invagination and forms a strong bond as it resorbs and is replaced by natural bone. It is a homogenous mixture of the graft crystals in a bovine Achilles tendon collagen matrix. The clusters are intertwined and form a hydrophilic matrix that absorbs blood. The material is initially radiolucent on placement but becomes radiopaque when bone turnover occurs over time and is eventually replaced by host bone. In socket preservation procedures using allograft material, it is essential to protect the graft from invagination of epithelium. Without a separate protective membrane, the grafting procedure becomes unpredictable. The Osteogen plug contains the graft material, but it also controls any connective migration through both a physical and chemical barrier. The physical barrier is created as the material is firmly compressed into the defect. Epithelial cells grow over the top rather than into the condensed material. As bleeding occurs, the crystals hydrate with blood and the resorption process begins with release of calcium ions and bone formation. (8,9)
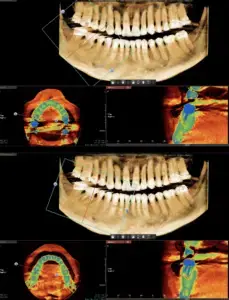
Here we will describe a novel approach to treat the cleaned out apical portion of a reappearing infected area on a mandibular first molar. Proper root canal treatment was completed years ago, but a fistula arose resulting in acute pain to the patient. (Figure one) Illustrates the typical radiolucency around the apex of an infected mandibular first molar. A draining fistula concerns the patient who has acute discomfort in the area. (Figure 2) A tissue reflection is made exposing the granulation around the apices of the mesial and distal roots. (Figure 3) A curette is used to remove the purulent growth completely and a small portion of root structure is eradicated. (Figure 4) Osteogen graft material (Impladent) is packed into the defect and condensed firmly without crushing. (Figure 5) A sheet of the same Calcium Apatite graft is positioned to the facial of the imperfection and will act as addition membrane barrier to prevent invagination of epithelium into the horizontal socket. (Figure 6) The post-operative radiograph in Figure 7 illustrates that the material has initial radiolucency. Sutures are removed in one week. The four-month post-operative view illustrates heathy attached gingiva, elimination of discomfort and removal of a fistula. (Figure 8) A digital radiograph confirms in two dimensions the healing over of the fistula tract. (Figure 9) Figure shows a two year follow up CBCT analysis indicates new bone formation in the defect area, allowing for retaining of then natural tooth in function. (Figure 10)









Retaining natural teeth has always been a goal for the profession. Dental implants have a positive long-term prognosis and provide function and aesthetics. Trying to salvage infected dentition with root canal therapy is a conventional treatment option. When this therapy is not successful due to inadequate or improper fill, fracture of the underlying root structure, or any number of idiopathic causes, the decision is made to retain the tooth or extract, graft with dental implant placement followed by integration and fabrication of implant retained crowns. In the past, apicoectomies attempted to save the tooth, eliminate the apical lesion, and retain natural tooth function. Here a novel approach to filling the defect created by the apicoectomy is discussed using a synthetic graft material. This material provided a framework for new bone formation and closure of the fistulous tract.
REFERENCES:
- Ruskin, J. D., Morton, D., Karayazgan, B., & Amir, J. Failed Root Canals: The Case for Extraction and Immediate Implant Placement. J Oral Maxillofacial Surg, 2005. 63(6), 829-831.
- Tavares, W, Fonseca, F et al. 3D Apicoectomy Guidance: Optimizing Access for Apicoectomies. J Oral Maxillofacial Surg. 2020. Mar; 78(3) 537.
- Iqbal, M. K., & Kim, S. (2008). A Review of Factors Influencing Treatment Planning Decisions of Single-Tooth Implants versus Preserving Natural Teeth with Non-Surgical Endodontic Therapy. J Endod. 2008. 34(5), 519-529.
- Walivaara, DA, Abrahamsson, P et al. Periapical Tissue Response After Use of Intermediate Restorative Material, Gutta Percha, Reinforced Zinc Oxide Cement, and Mineral Trioxide Aggregate as Retrograde Root End Filling Materials: A Histologic Study in Dogs. J Oral Maxillofacial Surg. 2012. Sept; 70(9). 2041-7
- Bodrumlu, E. Biocompatibility of Retrograde Root Canal Filling Materials: A Review. Aust Endod J. 2008. Apr; 34(1), 30-35.
- Badr, A. Marginal Adaptation and Cytotoxicity of Bone Cement Compared with Amalgam and Mineral Trioxide Aggregate as Root-end Filling Materials. J Endod. 2010 Jun; 36(6).
- Cochran, D. Rationale for the Application of the GTR Principle Using a Barrier Membrane in Endodontic Surgery: A Proposal of Classification and Literature Review. Int J Perio Rest Dent. 2001. 21, 127-139.
- Kosinski, T. Simple and Predictable Socket Preservation Techniques All Dentists Can Implement Regardless of Extraction or Grafting Experience. The Profitable Dentist, Summer 2016.46-50.
- Kosinski, T. A Simple and Cost-Effective Socket Preservation Technique. DentalCEToday.com. April 2016.
About co-author, Dr. Stephanie Tilley
Dr. Tilley is a graduate of the University of Alabama School of Dentistry. She is a native of Pensacola, Fla, and has been practicing dentistry in her hometown since 1998. She keeps up with the latest in dentistry by attending continuing education seminars on topics such as oral surgery, implants, veneers, periodontal disease, cosmetic procedures, and much more. Dr. Tilley has also done extensive training at the Las Vegas Institute for Advanced Dental Studies and the Engel Institute with Drs. Timothy Kosinski and Todd Engel. Her lectures discuss bone grafting procedures and surgical and prosthetic aspects of implant dentistry. She is a Fellow of the International College of Dentists, the American College of Dentists and the Academy of Dentistry International. Dr. Tilley is member of the AGD, the ADA, the Florida Dental Association, the Alabama Dental Association the Academy of Laser Dentistry, and the Academy of American Facial Esthetics. Dr. Tilley is also a Fellow with the International Congress of Oral Implantologists. She has been featured in several national dental publications and has published extensively on implant dentistry techniques, lasers, and Botox/ fillers. She can be reached via email at stephflynntilley@cox.net.